Aged Care
Aged care service support for healthcare providers in Western & Far West NSW
At Western NSW Primary Health Network (WNSW PHN), aged care is a key priority. We are committed to supporting healthcare providers to deliver high-quality, coordinated care for residents living in residential aged care homes (RACHs).
Our goal is to reduce avoidable hospitalisations and improve health outcomes for older people by:
- Expanding access to telehealth services
- Supporting after-hours care planning and service delivery
- Facilitating access to GP-led services within RACHs
We understand the unique challenges faced by providers working in aged care. That’s why we offer resources, programs and tailored support to help you navigate these complexities and enhance the care you provide.
To learn more about the aged care services and initiatives we fund in the community, visit our Services We Fund page.


Explore our aged care initiatives for RACHs
We offer a range of aged care initiatives designed to support RACH providers in our region:
Yellow Envelope
A tool designed to facilitate the safe and person-centred transfer of RACH residents to and from hospital.
ISBAR
A simple communication tool to support effective conversations in healthcare settings, ensuring critical information is conveyed clearly.
Residential Aged Care After Hours Plans
Resources, templates, and support for after-hours care in RACHs. Please contact us on agedcare@wnswphn.org.au.
Digital Health Solutions for Residential Aged Care
Access CPD-endorsed telehealth training to help aged care staff provide safe, effective virtual care.
How to make referrals to My Aged Care
Use the following methods to refer patients to My Aged Care.
- Online Referral via GP Practice Software: Use the Make a Referral page on the My Aged Care website to complete the online form and add any relevant attachments.
- Phone Referral: Call 1800 200 422 (8am–8pm weekdays, 10am–2pm Saturdays). Patients don’t need to be present, but their consent is required.
For more information on referrals, visit My Aged Care.

electronic Palliative Approach Framework (ePAF)
The Palliative and End of Life Model of Care is an individualised yet standardised needs-based approach for the care of patients with life-limiting disease in the last year of life. This electronic Palliative Approach Framework (ePAF) aims to assist carers and healthcare professionals to assess, plan and care for patients with advancing life-limiting illness.
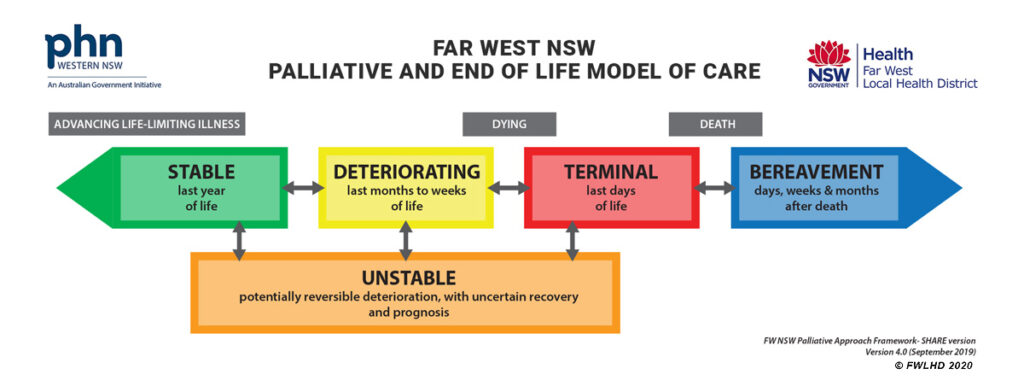
This project is funded by the Department of Health, Disability & Ageing under the Primary Health Networks Greater Choice for At Home Palliative Care.
